For anyone who thinks Greater Cincinnati's heroin epidemic is about as bad as it could get, consider the catastrophe in Scott County, Indiana.
The rural community two hours from Cincinnati made international news when public health officials discovered an HIV outbreak the likes of which nobody had ever seen.
Scores of intravenous drug users in the county's tiny city of Austin got the virus that causes AIDS from sharing and re-using dirty needles, cotton and cookers. Since the start of the outbreak, 210 people in Scott County have been diagnosed with HIV, and most are concentrated in Austin, which has a population of fewer than 2,500. Nearly 95 percent of the infected also have hepatitis C.
The Tri-State's heroin epidemic makes it ripe for a crisis just like the one there -- only bigger.
Dr. Lynne Saddler, the Northern Kentucky Health Department's district director, estimates that if the region were to have an outbreak the scale of Scott County's, it would result in 3,000 new HIV cases with a lifetime cost of care topping $1 billion.
"We're sitting on a potential time bomb," said Dr. A. George Smulian, director of the infectious disease division at University of Cincinnati. "And we have to do our best to try and diffuse it."

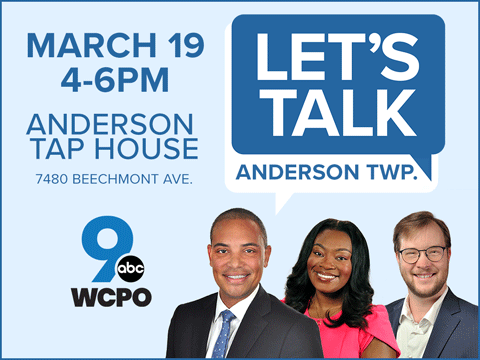
For much of the past year, WCPO has studied the HIV outbreak in Scott County, population 24,000, talking to doctors and nurses, addicts and activists, in an effort to find lessons that might help Greater Cincinnati avoid the calamity that befell our neighbor to the southwest. All the while, doctors and public health officials here have been doing the same thing.
The Northern Kentucky Health Department is putting a real-time HIV surveillance system in place to get information about a potential outbreak as quickly as possible, and the department expects to complete a comprehensive HIV outbreak response plan in the coming weeks. UC already is monitoring occurrences of the diseases and infections that increased in Scott County in the years and months leading up to the outbreak.
Still, there is only so much anyone can do in the face of an IV drug epidemic that shows no signs of slowing. And there are those here who worry that Scott County could offer a stark preview of Greater Cincinnati's future.
"It's devastating," said State Rep. Terry Goodin, a Democrat from Austin. "It's going to be difficult for the community to bounce back."
'It was Insane'
News of the HIV outbreak in Scott County broke in early 2015. The sparsely staffed health department there had never handled HIV cases before then. Instead, the regional Sexually Transmitted Diseases Department in Clark County had handled all cases of HIV. The system made sense at the time.
After all, Scott County had fewer than five new cases of HIV annually before the outbreak, said Brittany Combs, Scott County's public health nurse.
But the Clark County department detected an alarming spike. A pregnant woman who was an IV drug user had a routine HIV test at a local hospital that came up positive. Everyone in her household got tested as a result, and all of them were HIV positive, too.
"Since needles were not available at all at that point, everybody shared with everybody," Combs said. "It was insane what people would do."
An opioid pain medication called Opana was the drug of choice in Scott County. People abusing the powerful painkiller typically crushed it, mixed it with liquid and then injected it.

The IV drug use wasn't a surprise to public health officials. Rates of hepatitis C had been on the rise in Scott County for years, and everyone assumed that was linked to IV drugs, Combs said.
But HIV was something else.
"You look in Scott County, and we have people in their young 20s being diagnosed," said Dr. Jerome Adams, Indiana's state health commissioner.
It has been more than 30 years since a 13-year-old Indiana boy named Ryan White was diagnosed with AIDS following a blood transfusion. He became the face of the devastating disease in the 1980s and inspired the federal 1990 Ryan White Comprehensive AIDS Resources Emergency Act.
But all that happened before many of the young people infected in Scott County were even born. The public there thought of HIV and AIDS as sexually transmitted diseases, spread mostly by men having unprotected sex with other men.
"We had to educate a whole generation of folks from the ground up," Adams said. "What HIV is, what the risk factors are."
Health care providers in Scott County had to educate themselves, too. Not about HIV, but about addiction and the measures they needed to put in place to try to stop the spread of the virus in the community.
A public health disaster
"Everything happened so quickly," Combs said. "The state department of health called in preparedness teams like when a tornado happens. Because this was a disaster."
State and local officials established "one-stop shops" so people could get copies of the birth certificates and photo IDs they needed to sign up for insurance, along with mental health counseling and information about rehab centers.
But the turning point happened a couple of months into the outbreak when Vice President-elect Mike Pence, Indiana's conservative Republican governor, signed an executive order that allowed Scott County to start a needle exchange.
Combs was skeptical of the approach at first.
"Even as a nurse, I didn't understand substance abuse the way I should have," she said. "Even we at the health department were like, 'we're not going to do that -- that's enabling users.'"
Combs said after studying the research she realized that the needle exchange was her hometown's best hope.
Once the exchange began, it opened her eyes to how widespread IV drug use had become. She recalled one of the early days of the exchange when she helped a 20-something young man who was waiting at the health department with his mother and grandmother.
"He looked over at his mother and said, 'Hey Mom, what size needle do we like?'" she said. That's when Combs realized they all shot up opioids together. "It's so multi-generational."
The needle exchange program also has connected many people to the health department for the first time, and they are starting to get other ailments addressed, too.
"I call them walking medical disasters. It's been years and years since some of them have ever been to a doctor," Combs said. "They're just people, too. And they need help."
Help in Scott County also has come in other forms.

Social worker Michelle Korty received a grant to try to reduce the further spread of HIV by providing counseling to women in recovery and those who are sex workers. The women are regularly tested for HIV, and Korty and the colleague who runs the program with her make sure any of them who aren't infected are taking PReP, or Pre-Exposure Prophylaxis. That's the daily use of anti-HIV medication to reduce the chances that people at high risk of getting HIV will become infected.
For those who are infected, the virus has been "a wakeup call," said Korty, who operates a counseling center called A Place to Be. Many of the women in recovery and sex workers she counsels became homeless after they were diagnosed, she said, because the people they were living with didn't want HIV in the household.
"These are women who have lost everything, including their children, who have been lost to the system," Korty said. "You have to deal with that, the grief and the loss that all of the drugs took care of before."
Hooked and hopeless
Scott County doesn't have any homeless shelters, Korty said. So losing a place to stay often means sleeping outside.
Michael McIntosh knows all about that.
He lived on the street after he got out of prison in May. McIntosh became addicted to opioids years ago after six of the discs in his back were crushed in a bad car wreck.
He got an Oxycontin prescription for the pain and couldn't get enough of it. Eventually he started shooting up Opana and then got hooked on heroin. The addiction cost him his job, his marriage and his kids. After prison, he walked the streets day and night, searching for his next high.

"There's a few times that they found me in a ditch face down because I was so high," he said.
Life turned around for McIntosh when he wandered into Food 4 R Souls at Church of the New Covenant in Austin. Each week volunteers there serve up a warm welcome and a hot meal to anyone who walks through the door.
"They didn't see you as you're strung out, you're this drug addict, this worthless human being, like most people do," McIntosh said.
McIntosh was so moved that he asked Assistant Pastor Paul Thomas to pray with him one evening and was baptized that same night.
"The stronger I've built my faith, it's like my body is healing itself," he said. "The walk with God has just been so incredible."
McIntosh said he had been off opioids and the needle for two months when he talked with WCPO. And despite years of IV drug use, he had never come up positive for HIV in all the times he was tested.
"I never used after anybody, and I never used a needle more than once," McIntosh said.
Still, he has plenty of friends in Austin who have HIV. They're so addicted to the drugs and the needle, he said they figure the disease is part of the deal.
"They say, 'If you ain't HIV'in, you ain't livin,'" McIntosh said. "It's sad. It's heartbreaking."
He says that because he has been there. He knows the powerful pull that opioids can have and how difficult it can be to walk away from the drugs that make the pain go away.
But McIntosh knows most people don't feel that way.
"The community's so hard on anybody and so judgmental," he said. "If somebody does try (to quit), they're still being judged for what they've done."
The slow creep
Scott County has organizations working to reduce the stigma surrounding drug addiction and mental illness.
The community now has recovery groups that meet every night of the week. Before the HIV outbreak, the county didn't have any support groups for people trying to beat their addictions, said Lori Croasdell, coordinator for the Coalition to Eliminate the Abuse of Substances of Scott County.

"Some people don't even believe that it's a disease," Croasdell said. "They believe that it's a choice, and they haven't educated themselves on the fact that it is a brain disease and a chronic illness."
Scott County and its 24,000 residents remain divided. Many in the more affluent city of Scottsburg see the HIV outbreak as an Austin problem, she said.
"Nothing could be further from the truth," Croasdell said. "This is a struggle our entire county has."
The community has been worn down by the negative publicity. She said business leaders have asked her to stop talking so much about the HIV problem "because it's just killing business."
That's a concern for Goodin, the state lawmaker, too.
"As Scott County moves forward, it's tough as businesses look at an area to move into with corporations or factories," Goodin said. "It's tough for those folks to look at an area of heartache and say, 'we're going to go there.'"

But that's exactly what state economic development officials must encourage for the community to heal, he said.
A lack of jobs and hope made Austin ripe for IV drug use to start with, and the problem spread quietly for years.
"It just crept so slow and so long. It's kind of like that dandelion that grows up in your yard," Goodin said. "The first day you see it. But then, after a while, you don't necessarily see it anymore."
Perhaps the scariest part, though, is that the same risk factors that led to Scott County's HIV outbreak are common in communities across the country.
"People often ask me what's unique about Scott County," said Adams, the Indiana health commissioner. "I tell them, 'Absolutely nothing.'"
'HIV will inevitably follow'
The U.S. Centers for Disease Control and Prevention underscored that fact with a May report that identified 220 counties out of 3,007 nationwide as being at risk for an outbreak of the virus that causes AIDS.
Kentucky has 54 counties among those 220, making it the most vulnerable state in the nation for an HIV outbreak.
In Northern Kentucky, Grant and Gallatin counties both are on the list. Nearby, Dearborn, Switzerland and Ripley counties in Indiana are on the list, too.

"That report really put even more pressure on the community," Saddler said. "Then it wasn't just us -- the local health department -- saying we are at risk."
So far, reported cases of HIV have been steady in Northern Kentucky and Hamilton County.
But public health officials on both side of the river are keeping close watch on rates of hepatitis C, which was a warning sign before the HIV outbreak in Scott County.
In 2014, Northern Kentucky had one of the highest rates of acute hepatitis C infection in the country, according to Northern Kentucky Health Department data. That's a short-term illness that occurs within six months of being exposed to the virus. And cases of non-acute hepatitis C -- the long-term illness that can lead to serious liver problems -- have increased every year from 2006 through 2015.
Cases of hepatitis C also have been on the rise among people between the ages of 24 and 35 in Hamilton County, said Hamilton County Public Health Commissioner Tim Ingram.
"Right now hepatitis C does concern us," Ingram said. "But our HIV rates are stable. I hope they stay that way."
Linda Seiter worries those rates could be artificially low because there are IV drug users locally who refuse to get tested for HIV.
Seiter is executive director of Caracole, a Northside-based nonprofit organization that provides HIV prevention and testing for the community along with affordable housing and case management for people living with HIV and AIDS.
Caracole staff members do hepatitis C and HIV testing as part of the Cincinnati Exchange Project, a syringe exchange that started in early 2012. And some IV drug users who take part in the exchange won't agree to be tested for HIV because of the stigma that still is associated with the virus, Seiter said.
"We already have the heroin epidemic. We already have the spike in hepatitis C," Seiter said. "Why would we believe this community would be any different? HIV will inevitably follow."
Seiter has other reasons to worry, too.
A troubling trend
A Caracole housing program for homeless people with HIV has admitted 27 new residents so far this year. Of those, more than half either injected drugs themselves or had lived with someone who injected drugs and believed they contracted the disease through IV drug use.
That's a small percentage of the roughly 1,500 people with HIV or AIDS who count on Caracole for housing and other services, the vast majority of whom contracted HIV by having unprotected sex, she said.
But it's a troubling trend.
"We're very concerned about that -- that this is the top of the iceberg," she said. "I feel like we're behind."

It took five years for advocates to get Ohio state laws changed and approvals from local governments to start the Cincinnati Exchange Project, which now exchanges 10,000 syringes each month at four different sites each week.
The Kentucky General Assembly passed legislation in 2015 allowing for syringe exchanges in the commonwealth. Saddler said she believes the crisis in Scott County helped convince lawmakers who had been unsure about the measure in prior years.
Still, Northern Kentucky's only syringe exchange project in operation is in Grant County. Officials in Kenton County and the city of Covington have agreed to allow a syringe exchange there, too, but the Covington location won't be permitted to open until at least one additional syringe exchange is operational in the region the Northern Kentucky Health Department serves, Saddler said.
The longer it takes to get such programs in place, the more likely it is that police officers, firefighters and kids will come across infected syringes left on playgrounds or in alleys. Those bad encounters can leave people infected with a disease they will have to manage for the rest of their lives.
"It puts us all at risk," Seiter said.
That gets to what might be the most important lesson of all to come from Scott County: The opioid epidemic already reaches far beyond the families lost in the drug's fog and has the potential to reach farther still.
The community must approach drug addiction as a disease not "a moral failing," as Indiana's Dr. Jerome Adams put it.
People addicted to heroin must be able to trust health care providers in order to get the medical treatment and counseling they need to resume their places as productive members of society.
And public health officials must advocate for what works best while continuing to prepare for the worst.
In the words of UC's Smulian: "Hopefully we can avoid it. And it won't just be a matter of time."
WCPO Digital Reporter Lucy May and Photojournalist Emily Maxwell spent much of 2016 researching the HIV outbreak in Scott County, Indiana, to find lessons for Greater Cincinnati and Northern Kentucky in the aftermath of the crisis. Dave Niinemets was the editor for this project.